Every morning, different health facilities in Uganda’s island districts and border communities begin their normal routine of treating patients. Many of these patients are girls and women arriving with severe complications arising from unsafe abortions and in urgent need of Post-Abortion Care (PAC).
In Kalangala district (Ssese Islands), a 20-year-old Sarah (not real name) is lying on a small bed at Kalangala Health Centre (HCIV), recovering from a critical condition.
She arrived at the facility frail and frightened after an unsafe attempt to get rid of a pregnancy (abortion). But her life is no longer in immediate danger as doctors and midwives worked tirelessly to revive her condition.
Sarah, originally from Mubende district, was promised a hotel job in Kalangala but forced into sex work, where repeated sexual assaults led to an unwanted pregnancy. She later sought an unsafe abortion which caused serious internal complications.
Like many young women across the country, Sarah delayed seeking professional medical help out of fear of arrest or being stigmatised and questioned at the health facility, which worsened her health condition.
However, she received PAC emergency treatment, and the health workers’ main concern was stabilising her and saving her life. Similar situations keep happening across the country. The teenagers and women keep falling severely sick with life-threatening complications after carrying out unsafe abortions which require PAC.
Across districts in the Greater Masaka Region, young girls, including those with disabilities, often get stranded when trying to go for PAC, especially after unsafe abortions linked to sexual violence and coercion. They often arrive too late at the health facilities when their health is in a critical state, due to fear of being stigmatised, judged or arrested.
These cases clearly show how restrictive laws keep pushing girls and women into unsafe methods of terminating unintended pregnancies. This further increases the burden on the free but still costly PAC services in the country.
Just because the safe abortion alternatives are limited, PAC remains a critical lifeline for thousands of girls and women each year. Uganda’s law tightly outlaws access to safe abortion under the Penal Code Act except for exceptional circumstances.
PAC Services, Public Health Crisis

The World Health Organisation (WHO) estimates around 73 million induced abortions take place globally each year. In Uganda, the legal restrictions on safe abortion have further pushed many to opt for underground procedures, which sharply increases the risk and demand for PAC services.
Dr. Frank Kasirye, the Maternity In-Charge at Kalangala Health Centre IV, explains that 31 people reported for PACs between April and June 2025. “Many patients, especially from far islands and landing sites, struggle to get timely and specialised care for such complicated cases,” he explains.
However, he adds, abortions are reducing among school children but are still persistent among commercial sex workers. According to Kasirye, most costs of PAC arise from treating incomplete abortion. “A significant proportion is spent treating more patients with serious complications, such as sepsis, lacerations and perforations,” he states.
Robert Ssebalamu, the Community Health Extension Worker (CHEW) in Kalangala, says that he registers an average of 11 to 12 girls every month, in need of PAC and refers them to different health centres, including the HCIV.
According to Anastazia Nassali, a midwife at Kalungu HCIV, the delays in seeking PAC primarily happen out of fear of being arrested or stigmatised.
The situation is even worse in remote villages where transportation is difficult to find, health facilities are far away and getting medical care is expensive. She further adds that at least three women go for post-abortion care services every month, and the majority are being saved from severe complications.
Dr. Moses Nkanika, the Lyantonde District Health Officer (DHO), reveals that many abortion cases are never reported because the survivors fear being stigmatised or criticised by religious leaders.
“In the last two years, at least 622 people have come for post-abortion care services – 337 in 2024 and 285 this year,” he explains, adding that sensitisation campaigns are needed for people to know these services are available and free.
According to Maria Nagujja, the In-charge of Maternity at Kalisizo Hospital in Kyotera district, more than 180 people have gone for post-abortion care services. These numbers reflect how many people risk their lives to use unsafe procedures because safe abortion services are restricted by law.
Police crime report 2024
| The Uganda Police Force registered 728 abortion cases between 2019 and 2024, according to the 2024 Annual Crime Report. 2020 had 396 cases, becoming the highest number in six years. In 2019, 68 cases were recorded, 2021 (56), 2022 (59), 2023 (81) and 2024 (68). |
The same report indicates that the Greater Masaka Region recorded 951 sex-related cases, with Kyotera, Lwengo and Sembabule recording the highest number of cases.
NGOs, Activists speak
Patricia Namiwanda, the Sexual Reproductive Health and Rights (SRHR) and Youth Development Officer, at the Association of Disabled Persons Living with HIV and Tuberculosis (TB) in Uganda (ADPHA-Uganda), says many teenage girls with disabilities largely face limitations in accessing timely PAC and vital information about SRHR.
Gloria Namyalo, an experienced Social Worker in Masaka district, says many teenage abortions are carried out with the help of untrained Traditional Birth Attendants (TBAs), increasing the risk of serious complications and PAC demand.
CEHURD, HRAPF Petition
On 14th November 2025, the Centre for Health Human Rights and Development (CEHURD) and the Human Rights Awareness and Promotion Forum (HRAPF) received the long-awaited judgement in their Constitutional Petitions (No. 25 of 2020 and No. 10 of 2017) on termination of pregnancy in Uganda.
The petitions were challenging the State’s failure to formulate and enact a law regulating the termination of pregnancy in Uganda, in line with Articles 22(2) and 79(1) and (2) of the 1995 Constitution.
However, the minority decision affirms what evidence, constitutional values, and medical realities have consistently shown: that the criminalisation of abortion endangers women’s lives, violates their dignity, undermines their right to health, and contradicts Uganda’s obligations under national and international human rights law.
CEHURD further criticises the court’s position for ignoring the plight of the many girls and women facing defilement, incest and rape, evidenced by national documents such as the annual police crime reports.
According to Rhodine Kitandwe, a Health Rights champion and lawyer at CEHURD, unsafe abortion remains one of the leading causes of maternal deaths resulting from severe complications such as sepsis and haemorrhage, among others.
Kitandwe explains that the dangers are intensified when infectious diseases are part of the picture, because pregnancy weakens a prospective mother’s immune system, and the risk of opportunistic infections rises.
Uganda has made significant progress in reducing maternal deaths, currently estimated at 189 per 100,000 live births (2022). However, this figure is still far above the SDG 3.1 target of 70 per 100,000 live births.
Another Human Rights Lawyer, Susan Baluka, says there is apparently no legal protection for vulnerable groups, especially teenagers and PWDs, who remain at high risk with PAC as the main option for immediate medical treatment.
Obstetrics/Gynaecology Specialist
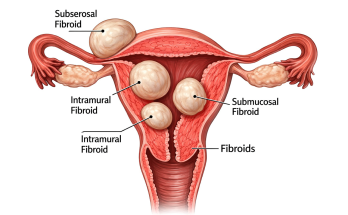
Dr. Simon Peter Kayondo, an obstetrician-gynaecologist specialist, says that excessive bleeding commonest complication and the leading cause of death associated with unsafe abortion, especially among young girls and women. Other short-term complications include post-abortion infections and injuries to the internal organs that are common with unsafe procedures.
However, Kayondo, also the Vice President of the Association of Obstetricians and Gynaecologists of Uganda (AOGU), warns that long-term effects that may emerge later (months or years) include infertility whereby the unsafe abortion survivors may struggle to conceive, the damaged uterus or cervix that can increase the risks of complications in future pregnancies, in addition to chronic pain, psychological distress among others.
According to Kayondo, PAC involves various medical steps designed to address emergencies and prevent future unwanted pregnancies and repeated abortions.
However, he adds, the legal restrictions affect the operations of health workers in various ways. Some health workers struggle to determine who qualifies for lawful abortion and who doesn’t.
“As a result, some patients, who would ideally qualify for safe abortion services, still resort to unsafe procedures because many health providers are uncertain about the law,” he says.
Asa result, the uncertainty has continuously created persistent tension among the providers. “Some health workers are caught in the traps of the law while offering PAC. It is easy for someone to accuse them of offering an abortion when they are actually offering PAC,” he adds.
“In medical practice, the procedures used for safe abortion and PAC are often the same and quite difficult to distinguish. So, it is challenging to distinguish them, creating an ethical and professional dilemma,” he states.
As Uganda considers whether to reform its abortion law, experts and health professionals argue that the consequences of doing nothing are already felt in hospital wards across rural areas, island communities and border towns.
Unless the legal and health system reforms are addressed, unsafe abortion will continue to raise the demand for PAC in Uganda.
This story was produced with support from a reporting grant provided by AKINA MAMA WA AFRIKA (AMWA).